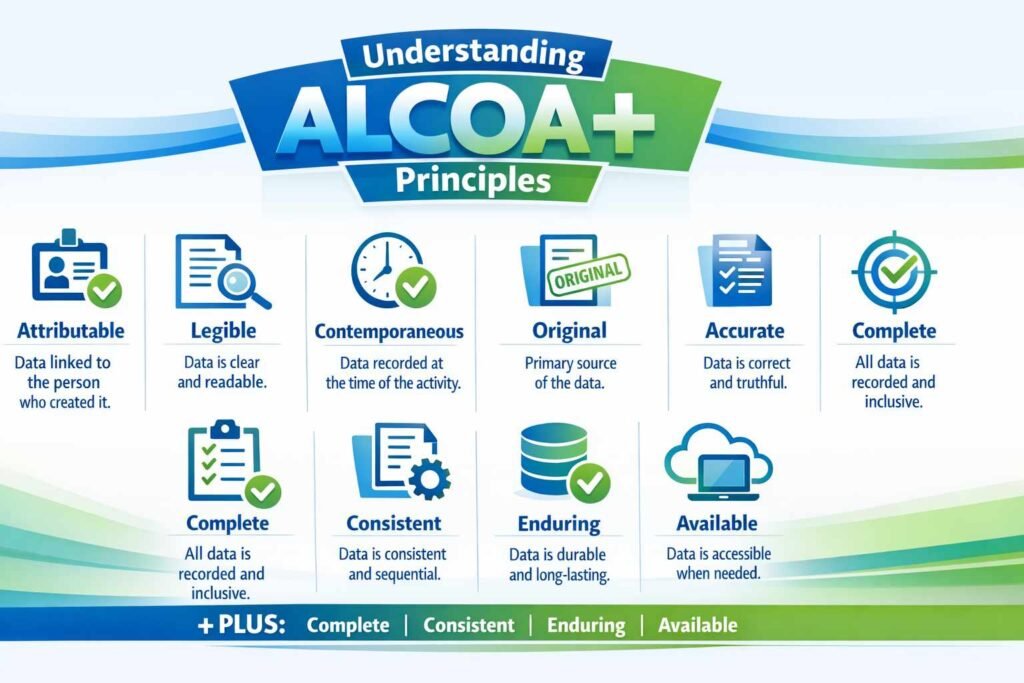
ALCOA stands for Attributable, Legible, Contemporaneous, Original, and Accurate—the five fundamental data integrity principles established by the FDA in the 1990s to ensure pharmaceutical data quality and regulatory compliance. These principles form the cornerstone of Good Documentation Practices (GDP) and Good Manufacturing Practices (GMP), creating a framework that guarantees every piece of data in your pharmaceutical operations is trustworthy, traceable, and tamper-proof.
In regulated industries including pharmaceuticals, biotech, medical devices, and clinical research, ALCOA compliance isn’t optional—it’s mandatory. A single data integrity failure can result in rejected regulatory submissions, costly product recalls, or enforcement actions by the FDA, EMA, or other regulatory bodies. Today’s pharmaceutical professionals must understand not just ALCOA, but also its evolved versions: ALCOA+ and ALCOA++, each representing increasingly sophisticated approaches to data governance in the digital age.
THE 5 CORE ALCOA PRINCIPLES EXPLAINED
1. Attributable – Who Did It, When, and Why?
The Attributable principle establishes complete accountability by ensuring every data entry, change, or action can be traced to a specific individual with a timestamp. This principle answers three critical questions: Who performed the action? When did it occur? What was completed?
Technical Implementation:
- Unique user identifications for every data entry (no shared login credentials)
- Automatic capture of user ID, timestamp, and action type in audit trails
- Electronic signatures linking individuals to specific records or approvals
- Complete traceability preventing anonymous entries or modifications
Pharmaceutical Example:
In a GMP batch record, every temperature reading, weight measurement, and quality control result must be attributed to the technician who recorded it, the exact time of recording, and the instrument used. If a technician later reviews the record, that review action is also logged with its own timestamp.
Regulatory Expectation (FDA 21 CFR Part 11):
The FDA expects that electronic records clearly identify the individual responsible for each entry, making it impossible for data to exist without a documented author.
2. Legible – Readable and Permanent
Legible data must be readable and permanent throughout its entire lifecycle, from initial creation through archival and eventual destruction. This principle applies equally to paper records and electronic systems.
For Paper Records:
- Use of indelible ink (ballpoint pen) rather than pencil
- Corrections made with a single strikethrough line, allowing original entry to remain visible
- Permanent binding preventing page removal or insertion
- Storage in controlled environments protecting from moisture, fading, or deterioration
For Electronic Records:
- Human-readable metadata stored alongside electronic data
- Prevention of data corruption or loss during system migrations
- Version control ensuring current and historical records remain accessible
- Format stability ensuring records remain readable even if original systems become obsolete
Pharmaceutical Example:
A handwritten batch record cannot use erasers or white-out; corrections require a single line striking through the error, initials, date, and reason for change. Electronic laboratory information management systems (LIMS) must maintain audit trails showing all versions of results, with timestamps and human-readable explanations for any corrections.
3. Contemporaneous – Recorded at the Time of Activity
Contemporaneous recording means data must be recorded at the time the activity occurs, not retrospectively. This principle prevents fabrication and ensures records reflect real-time observations and decisions.
Why Contemporaneous Recording Matters:
- Memory decay: Recording data hours or days later invites errors, approximations, and unintentional omissions
- Fabrication risk: Retrospective entries cannot verify that the activity actually occurred as documented
- Regulatory position: FDA inspectors view post-hoc data entries as red flags for potential integrity violations
Pharmaceutical Example:
Temperature readings in a controlled storage area must be recorded at the time of measurement, not compiled at the end of the day from notes. If a batch release decision is made, the person making that decision documents their reasoning and approval at the time of release, not days later during record compilation.
Exception Protocol:
Some industries allow “nearest practical time” for safety reasons (e.g., surgical nurses documenting vital signs minutes after recording during emergencies). However, pharmaceutical documentation expects same-shift entries at minimum, with clear justification for any delay.
4. Original – First Capture or Certified True Copy
The Original principle requires that data be recorded in its first, original form—not as a copy or summary of another document. If copies are used, they must be certified true copies, verified and authenticated by authorized personnel.
Original Data Sources:
- Direct instrument output (laboratory analyzer printouts, temperature charts)
- Initial handwritten observations by qualified personnel
- Primary electronic records from validated systems
- Certified true copies bearing authentication by authorized individuals
Prohibited Practices:
- Transcribing data from informal notes into formal records (creates two versions)
- Creating batch records by compiling data from multiple sources without clear source identification
- Photocopying records without certification
- Summarizing raw data without maintaining the original dataset
Pharmaceutical Example:
A laboratory technician analyzes a sample using a HPLC instrument. The original data is the direct instrument output, time-stamped and electronically signed. That printout (or electronic record) is the original. If a summary report is later created for the quality review, that summary must reference the original data, but the original instrument output remains the legal record.
5. Accurate – Error-Free and Truthful
Accurate data is correct, complete, and honestly represents the actual result or observation. Accuracy requires that data be recorded without errors, falsification, or omission of relevant information.
Ensuring Accuracy:
- Double-checks or verification procedures (e.g., second technician confirming results)
- Defined acceptance criteria preventing ambiguous or estimated entries
- Root cause investigation of anomalies (unusual results must be investigated, not ignored)
- Correction procedures with clear justification for any changes
Pharmaceutical Example:
A Quality Control analyst obtains a dissolution result of 98.5% for a drug product. This is accurate. If the analyst later discovers a calculation error and the true result is 95.2%, they cannot simply erase the original entry. Instead, they document the correction with: the original result, reason for change, corrected result, date, time, and signature. The audit trail shows the entire history, maintaining accuracy and transparency.
Regulatory Implication:
The FDA expects that raw data accurately reflects what was actually observed or measured, not what the analyst thinks should have been observed. Rounding, estimation, or manipulation of results to meet specifications is a serious compliance violation.
EVOLUTION: FROM ALCOA TO ALCOA+ TO ALCOA++
ALCOA vs. ALCOA+ vs. ALCOA++: Comparison Table
| Principle | ALCOA (5) | ALCOA+ (9) | ALCOA++ (14+) |
|---|---|---|---|
| Attributable | ✓ Trace to individual | ✓ Enhanced audit trails | ✓ AI-monitored accountability |
| Legible | ✓ Readable, permanent | ✓ Format-stable archives | ✓ Cross-system accessibility |
| Contemporaneous | ✓ Real-time recording | ✓ Timestamped systems | ✓ Blockchain-compatible timestamps |
| Original | ✓ First capture | ✓ Source-verified originals | ✓ Immutable originals (digital) |
| Accurate | ✓ Error-free, truthful | ✓ Validated entry fields | ✓ AI-flagged anomalies |
| Complete | — | ✓ No deletions, all changes included | ✓ Data completeness algorithms |
| Consistent | — | ✓ Standardized format & sequence | ✓ Schema-enforced consistency |
| Enduring | — | ✓ Durable, tamper-proof storage | ✓ Cloud-encrypted, immutable records |
| Available | — | ✓ Easily retrievable | ✓ Real-time searchable systems |
| Integrity, Robustness, Transparency, Accountability, Reliability | — | — | ✓ Cultural, governance, digital-first |
What Is ALCOA+? The Four Additional Principles
Complete – Nothing Is Missing
Complete data means no deletions have occurred in the dataset. Every data point, outlier, failed attempt, correction, and revision must be preserved in the record.
Industry Problem ALCOA+ Solved:
Pharmaceutical companies were sometimes selectively excluding outlier results or failed batches from records, presenting only “good” data to regulators. ALCOA+ mandates inclusion of everything.
Implementation:
– All analytical results retained, including failed/out-of-specification batches
– Correction history preserved (original + correction visible together)
– Negative results documented alongside positive ones
– Audit trails showing every data state throughout the lifecycle
Regulatory Expectation:
FDA inspectors review data completeness extensively. Missing data points raise immediate concerns about intentional omission or cover-up.
Consistent – Standardized Format and Logical Sequence
Consistent data follows standardized formats, uses uniform terminology, and maintains logical sequencing that can be traced across the entire data lifecycle.
Examples of Consistency:
- Date formats (DD-MMM-YYYY) applied uniformly across all records
- Unit measurements (mg, %, IU) standardized per compound
- Approved abbreviations used consistently (not mixed with non-standard shorthand)
- Version numbering systematic (v1.0, v1.1, v2.0) rather than ad-hoc
Pharmaceutical Example:
A batch record for a tablet formulation includes dissolution testing at multiple time points. Each time point must follow the same format: time interval (e.g., “30 min”), specification range (e.g., “75–95%”), actual result (e.g., “87.3%”), and analyst identity. Consistency ensures that anyone—auditor, regulator, or future employee—can quickly understand the record without deciphering individual writing styles or interpretations.
Enduring – Durable, Tamper-Proof Storage
Enduring data must survive the entire data lifecycle on secure, validated systems that prevent loss, corruption, or unauthorized modification.
Durable Storage Requirements:
- Validated electronic systems (LIMS, ERP, document management) rather than temporary platforms
- Backup and disaster recovery protocols ensuring data survival
- Protected access controls preventing unauthorized alterations
- Long-term storage formats that don’t depend on obsolete technology
Pharmaceutical Example:
Batch records cannot be stored in temporary spreadsheets or emails. They must reside in validated pharmaceutical management systems with defined backup schedules, access logs, and retention timelines. If the company transitions systems (e.g., from one LIMS to another), data migration must be validated to ensure no loss or corruption.
Regulatory Concern:
During FDA inspections, regulators assess whether companies can retrieve 5, 10, or even 20-year-old records with complete integrity. Systems that cannot retrieve historical data face serious compliance findings.
Available – Easily Retrievable When Needed
Available data must be retrievable quickly during audits, inspections, or regulatory submissions. A record is only useful if the company can find and produce it on demand.
Accessibility Requirements:
- Documented search procedures enabling retrieval within defined timeframes
- Appropriate indexing (by batch number, product, date, etc.)
- System performance ensuring records load quickly
- Archived data accessible with same readability as current data
Pharmaceutical Example:
During an FDA inspection, a regulator asks to review all manufacturing records for Product XYZ from the past 3 years. The company must retrieve these records within hours or a single business day. Electronic systems with proper indexing can achieve this; paper archives stored haphazardly cannot.
ALCOA+ IN PRACTICE: Industry Applications
Where ALCOA+ Is Mandated:
Clinical Trials & Drug Development
- Case report forms (CRFs) must be complete, consistent, and source-verified
- Electronic data capture (EDC) systems enforce ALCOA+ through built-in controls
- FDA expects ALCOA+ compliance during clinical trial inspections
Manufacturing & Quality Control
- Batch records, testing records, and deviation logs must meet all nine principles
- Environmental monitoring data (temperature, humidity) requires ALCOA+ compliance
- Equipment qualification and validation records must be complete and durable
Supplier & Vendor Management
- Certificates of analysis (CoAs) from vendors must be original, not photocopied without certification
- Supplier audit records must be contemporaneous and traceable
- Quality agreements specify ALCOA+ expectations
Data Integrity Violations & Enforcement:
FDA’s 2015 warning letters emphasized ALCOA+ failures as a top compliance issue. Companies found guilty of:
- Selective deletion of data
- Retrospective record creation
- Unsigned or inadequately attributed entries
- Systems lacking complete audit trails have faced product recalls, consent decrees, and criminal prosecution in severe cases.
WHAT IS ALCOA++? The Next Evolution
ALCOA++ extends ALCOA+ by adding a governance and cultural layer, incorporating modern digital systems (cloud, AI, blockchain) and emphasizing organizational accountability.
ALCOA++ Additional Dimensions:
Traceable – Every action linked to individuals with complete audit trails, enabling post-hoc investigation of any anomaly or concern.
Transparent – Data practices are open, honest, and documented. Hidden manipulations or workarounds have no place in ALCOA++ culture.
Trustworthy – Systems and processes inspire confidence in data reliability, supporting regulator and patient trust.
Ethical – Data integrity embedded as a corporate value, not just a compliance checklist. Employees understand why data integrity matters.
Governance & Digital Integration – Cloud-based systems, AI anomaly detection, blockchain-compatible audit trails, and advanced data analytics integrated with ALCOA++ frameworks.
Who Uses ALCOA++?
Advanced pharmaceutical organizations and those preparing for future regulatory expectations (EMA and WHO are increasingly referencing ALCOA++ in guidance documents). Many global organizations are transitioning to ALCOA++ to maintain competitive advantage and demonstrate maturity to investors and regulators.
ALCOA COMPLIANCE: FDA 21 CFR Part 11 & Regulatory Framework
ALCOA principles are directly incorporated into the FDA’s regulatory foundation for electronic records:
21 CFR Part 11 Key Requirements:
- Systems must be validated to ensure accuracy and reliability
- Electronic signatures equivalent to handwritten signatures (requires secure authentication)
- Audit trails must be created and maintained automatically
- Records must be protected against loss, corruption, or unauthorized access
- Backup and archival procedures must ensure long-term accessibility
Global Regulatory Bodies Using ALCOA:
- FDA (USA) – 21 CFR Part 11, FDA Guidance on Data Integrity
- EMA (Europe) – ICH Q14, EMA Guidelines on Data Integrity
- WHO – WHO Technical Report Series and GMP annexes
- MHRA (UK) – UK GMP Annex 15, Qualification and Validation
- PIC/S (Pharmaceutical Inspection Co-operation Scheme) – GMP Guide incorporating ALCOA+
ALCOA IMPLEMENTATION IN PHARMACEUTICAL ORGANIZATIONS
Phase 1: Current State Assessment & Gap Analysis
- Data Inventory – Identify all data types (paper, electronic, hybrid), sources, and flows across the organization
- Gap Mapping – Assess existing processes against ALCOA+ requirements per regulatory framework
- Risk Assessment – Prioritize gaps by regulatory risk (manufacturing > administrative)
- Baseline Metrics – Document current compliance status for trending
Phase 2: System & Process Redesign
- Validated Systems Selection – LIMS, ERP, document management platforms meeting 21 CFR Part 11
- Data Entry Standardization – Design forms with predefined fields, dropdown lists, units, and validation rules
- Approval Workflow Integration – Embed electronic signature and routing into processes
- Audit Trail Configuration – Ensure automatic capture of user, timestamp, action type, and before/after values
Phase 3: Training & Culture Change
- Role-Based Training – QA, Manufacturing, R&D, Procurement staff trained on ALCOA+ expectations in their specific roles
- Documentation Practices – Establish and communicate SOP revisions incorporating ALCOA+ standards
- Leadership Engagement – Director-level commitment to data integrity culture, not just compliance
- Ongoing Awareness – Regular communications, case studies, and lessons learned
Phase 4: Monitoring & Continuous Improvement
- Compliance Metrics – Track audit trail completeness, corrections frequency, system uptime, data accessibility
- Internal Audits** – Quarterly review of sample records for ALCOA+ adherence
- Trending Analysis– Identify patterns (e.g., frequent corrections in one department) requiring intervention
- System Enhancement – Continuous evaluation of new features or tools improving ALCOA+ compliance
COMMON ALCOA VIOLATIONS & REMEDIATION
| Violation Type | Example | Regulatory Impact | Remediation |
|---|---|---|---|
| Missing Attributability | Shared login credentials; batch review without signature | Warning Letter risk | Implement unique user IDs, electronic signature workflows |
| Illegible Records | Faded ink, pencil entries, paper damage | Audit findings | Transition to validated electronic systems; paper form control |
| Retrospective Entry | Temperature readings compiled at end of week | 483 Observation | Implement real-time data capture; disciplinary action for employees |
| Non-Original Data | Photocopied CoAs without certification | Batch rejection risk | Require certified true copies; request electronic documents from suppliers |
| Inaccurate Results | Fabricated dissolution data to pass specifications | Consent Decree / Recall | Root cause investigation, corrective action, potential product recall |
| Missing Completeness | Outlier results excluded from batch record | Warning Letter risk | Retain all data; investigate and document outliers |
| Inconsistent Format | Date formats mixed (DD/MM/YY vs. MM-DD-YYYY) | System validation findings | Standardize data entry fields in validated systems |
| Lack of Durability | Records stored on obsolete systems; no backup | System failure = data loss | Migrate to validated, modern platforms with redundancy |
| Unavailable Data | Cannot retrieve records from 3 years ago during audit | Serious compliance finding | Archive data with documented retrieval procedures |
FREQUENTLY ASKED QUESTIONS ON ALCOA
What does ALCOA stand for?
ALCOA stands for Attributable, Legible, Contemporaneous, Original, and Accurate. These are the five foundational principles for pharmaceutical data integrity established by the FDA.
What is the purpose of ALCOA principles?
ALCOA principles ensure that all data in pharmaceutical operations is trustworthy, traceable, and suitable for regulatory submissions. They protect patient safety by ensuring that manufacturing and quality control decisions are based on reliable data.
Is ALCOA the same as ALCOA+?
No. ALCOA is the foundational framework (5 principles). ALCOA+ extends ALCOA by adding four principles (Complete, Consistent, Enduring, Available). ALCOA+ is now the industry standard and is expected by regulatory bodies during inspections.
When was ALCOA developed?
ALCOA was developed by the FDA in the 1990s as part of guidance on electronic records and electronic signatures (21 CFR Part 11). ALCOA+ was introduced later as regulatory expectations for data integrity evolved.
Is ALCOA compliance mandatory?
Yes, ALCOA compliance is mandatory for FDA-regulated pharmaceutical manufacturers. The FDA expects ALCOA+ compliance (not just ALCOA) during GMP inspections. Non-compliance can result in warning letters, product recalls, or enforcement actions.
What is the difference between ALCOA and ALCOA+?
ALCOA focuses on the five core principles. ALCOA+ adds four principles (Complete, Consistent, Enduring, Available) addressing modern pharmaceutical operations and digital systems. ALCOA+ is the current regulatory expectation.
What is ALCOA++ and who uses it?
ALCOA++ extends ALCOA+ by incorporating governance, ethics, and modern digital technologies. Advanced organizations and those preparing for future regulatory expectations use ALCOA++. WHO and EMA are increasingly referencing ALCOA++ in guidance documents.
How does ALCOA relate to 21 CFR Part 11?
ALCOA principles are incorporated into 21 CFR Part 11 (FDA’s regulation on electronic records and electronic signatures). Companies implementing ALCOA+/ALCOA++ inherently comply with 21 CFR Part 11 requirements.
Why is ALCOA important for clinical trials?
Clinical trial data integrity directly impacts patient safety and regulatory decision-making. ALCOA compliance ensures case report forms, laboratory results, and safety data are reliable and traceable, supporting FDA approval decisions.
What happens if we fail an ALCOA inspection?
FDA findings on ALCOA violations can range from 483 Observations (correctable within a set timeline) to Warning Letters (serious non-compliance requiring immediate remediation). Severe violations may trigger consent decrees, product recalls, or criminal prosecution.
Can small pharmaceutical companies achieve ALCOA+ compliance?
Yes. ALCOA+ compliance is required for all regulated pharmaceutical manufacturers, regardless of size. Small companies can implement compliant processes through validated systems (even cloud-based LIMS), strong SOPs, and training—often at lower cost than large enterprises.
How does ALCOA apply to paper records?
ALCOA principles apply equally to paper and electronic records. Paper records must use indelible ink, corrections must use single-line strikethrough, and records must be stored in secure, durable locations. However, electronic systems are increasingly preferred because they automate ALCOA compliance.
KEY TAKEAWAYS FOR PHARMA PROFESSIONALS
1. ALCOA is non-negotiable – Data integrity is foundational to patient safety, regulatory approval, and company reputation. FDA expects ALCOA+ compliance as the minimum standard.
2. Implement ALCOA+ (not just ALCOA) – The industry standard has evolved. Organizations that still operate under basic ALCOA face compliance risk. ALCOA+ addresses modern systems and regulatory expectations.
3. Systems enable compliance – Manual, paper-based processes struggle with ALCOA+ (particularly Contemporaneous and Available). Validated electronic systems (LIMS, ERP, document management) are essential.
4. Data integrity is cultural – Compliance requires buy-in from manufacturing floor to C-suite. Employees must understand why data integrity matters beyond “passing audits.”
5. Plan for ALCOA++ – While ALCOA+ is current regulatory expectation, forward-looking organizations are adopting ALCOA++ frameworks (cloud, AI, transparency) to maintain competitive advantage and prepare for evolving expectations.
6. Violations carry real consequences – FDA warning letters, product recalls, and criminal prosecution result from serious data integrity failures. The cost of non-compliance far exceeds investment in proper systems and training.
ADDITIONAL RESOURCES
- FDA 21 CFR Part 11: Electronic Records; Electronic Signatures
- FDA Guidance on Data Integrity: Investigation of Out-of-Specification (OOS) Test Results (2015)
- ICH Q14: Analytical Procedure Development
- WHO Technical Report Series: Annex 15 – Qualification and Validation
- USP <1058>: Analytical Data – Interpretation and Treatment (covers ALCOA+ in practice)
References
- FDA. Data Integrity and Compliance With Drug CGMP: Q&A (Final, Dec 2018).
- EU. Annex 11 – Computerised Systems. Public Health
- EMA. GMP/GDP Q&As; Guideline on Computerised Systems and Electronic Data in Clinical Trials (2023).
- WHO. TRS 1033 Annex 4: Guideline on Data Integrity (2021). WHO
- MHRA. GxP Data Integrity Guidance and Definitions (2018; page updated 2021).
- PIC/S. PI 041-1: Guidance on Data Integrity (2021). PicScheme
- Eurotherm ALCOA+ primer. Eurotherm
- Tulip Interfaces ALCOA guide (manufacturing). Tulip
- SCW.ai ALCOA+ guide / Digital Batch Record (features/examples). scw.ai
- Quanticate ALCOA++ (GCP/clinical focus). Quanticate
- ValGenesis best practices; DI by design. valgenesis.com
- OutsourcedPharma “Attributable” series & pitfalls. Outsourced Pharma
- 2025 GMP-compliance.org update noting ALCOA++ and copy definitions in EU context. ECA Academy